to see third part click here
to download full pdf CLICK HERE
to download full pdf CLICK HERE
acute non-suppurative Inflammation ; Catarrhal , serous, pseudomembranous, allergic, hemorrhagic inflammation (describing histopathology of each disease) l General pathology revision for dental student
II- Acute non- suppurative inflammation
- Increase
RBCs : hemorrhagic
inflammation
- Increase
fluid exudate : serous /
serofibrinous / Catarrhal
- Increase necrosis : Necrotizing - membranous - Allergic
Catarrhal inflammation
Definition :
- Mild acute
inflammation of ! M.M characterized by increase mucous
secretion.
Sites :
- M.M of R.T or GIT. ! best known example is ! common cold = coryza = Catarrhal rhinitis.
N/E :
- Mucus membrane is :edematous , congested , swollen and red & covered epithelium : 1st serous fluid then mucoserous then mucus.
M/E:
- Mucosal cells appear swollen due to mucous accumulation (mucoid degeneration) & may rupture or desquamate.
- Superficial parts of sub-epithelial tissue show hyperemia, inflammatory edema and mild neutrophil infiltration.
Fate :
- inflammation subsides & regeneration occur.
- 2ry infection e pyogenic bacteria (exudate becomes muco-purulent).
- chronic inflammation may lead metaplasia of surface
epithelium & fibrosis
of underlying tissue.
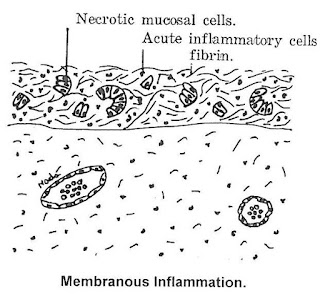
Membranous (pseudomembranous) inflammation
Def :
- Characterized by formation of membrane formed of fibrin, desquamated epith & inflamed Connective tissues.
Cause :
- Bacteria w have a low invasive capacity but grow on ! surface of mucous membrane & produce exotoxins as :
- Diphtheria
- Shigella (causing bacillary dysentry).
Site
- mucous membrane (M.M).
Pathogenesis:-
- Bacteria stick to the surface of the mucous membrane and releases exotoxin.
- The exotoxin produces superficial necrosis and acute inflammation of underlying tissue.
- As the exudate passes to the surface the fibrinogen in it clots & encloses the necrotic epithelium in fibrin network to form the pseudo membrane
- the
pseudo membrane contains
also the causal bacteria, neutrophils &erythrocytes (RBCs)
- Neutrophils accumulate at junction of living & dead tissue.
- Their digestive enzymes detach the membrane leaving a raw surface
- Toxemia
is evident
(as exotoxin is absorbed in the blood stream).
N/E :
- Early, mucous membrane is red with grayish yellow patches of necrosis. Next, patches coalesce to form diffuse slightly elevated membrane which is first adherent to underlying structures (due to rich fibrin content). If removed by force, it leaves a raw bleeding surface & it reforms again. Lymphadenitis of draining lymph nodes.
M/E :
1. Epithelium
: replaced by
pseudomembrane which contain :
- fibrin
network intangling in its meshes [
necrotic tissue , organism , inflammation cells ]
- necrotic tissue.
- organism
- inflammation cells.
2. Sub-epithelium
:
- The pseudomembrane: is formed of necrotic mucosal cells , bacteria, acute inflammatory
cells & excess fibrin. sub epithelial tissue shows features of acute inflammation; hyperemia, inflammatory
edema, excess fibrin & acute inflammatory cells specially neutrophils and
erythrocytes
Fate:
- Re-epithelialization
- Loss of mucosal glands & fibrosis.
Serous
inflammation
Serous inflammation
Def :
- Acute inflammation characterized by formation of increase fluid exudate rich in fibrinogen
- Acute inflammation characterized by increase watery fluid exudate.
Cause :
- It occurs more severe injuries & greater vascular
permeability allows passage of fibrinogen molecules.
Site :
- inflammation in serous sacs (pleura, pericardium & peritoneum).
- lung alveoli (lobar pneumonia).
- Skin as in herpes simplex & burn where watery vesicles are seen.
- Serofibrinous inflammation
Pathology :
N/E:
- Parietal & visceral layers become red, opaque, rough & thickened.
- Fine gray granules =
fibrin are seen on both internal surfaces.
- Serous fluid collects in the cavity
- According to proportion of serous fluid & fibrin.
- If ++ fibrin deposition è is of dry type.
- If ++ serous fluid collects in sac,è !wet type.
M/E :
- Serosa of visceral & parietal layers are swollen or desquamated
è bare surfaces.
- fluid exudate rich in fibrinogen from the bare surfaces è changes to fibrin network on both visceral & parietal layers entangling acute inflammatory Cells
- subserosa shows è hyperemia, edema & fibrin network enclosing the inflammatory Cellss.
Fate :
- repair by organization.
Hemorrhagic inflammation
Hemorrhagic inflammation
Def :
- Acute inflammation characterized
by vascular damage è hemorrhage
Cause
:
Cause :
- Severe injuries sufficient to cause vascular damage.
- Causative bacteria : Small pox, meningococci , strept. hemolyticus & Rickettsia.
Necrotizing inflammation
Def
Def
acute inflammation characterized by extensive tissue necrosis
Example
- Vincent’s angina and cancrum oris in the mouth
- Infective gangrene in the lungs
ALLERGIC inflammation
ALLERGIC inflammation
definition :
definition :
- A
type of inflammation in which the inflammatory reaction results
antigen / antibody reaction
- A type of inflammation in which the inflammatory reaction results antigen / antibody reaction
Course of acute inflammation depends on:
Course of acute inflammation depends on:
- type of tissue inflamed
- amount of tissue destroyed (w depends on the nature & severity of the irritant).
- type of tissue inflamed
- amount of tissue destroyed (w depends on the nature & severity of the irritant).
Fate of acute inflammation
Resolution :
- complete restoration of tissues to (N) normal
after acute inflammation.
- conditions that favor resolution are :
- Minimal or no cell death.
- Rapid removal of inflammatory exudate. e.g. Lobar pneumonia.
Healing by fibrosis.
After tissue destruction:
- In tissues
that can not regenerate.
- abundant fibrin or necrosis
Progression
to chronic inflammation
spread : death.








0 Comments