Dentin 1 (dentin structure) l Oral histology and biology MCQs for dental students
Dentin
Definition :
- Dentin is the mineralized tissue that forms the bulk of the
tooth.
Physical properties:
- Color: light yellowish.
- Hardness:
- It is elastic to provide
flexibility which prevent fracture
of the overlying brittle enamel.
- It is less hard than enamel, harder
than cementum and bone.
- Thickness: 3 -10mm or even more.
- Radiograph: more radiolucent than enamel, more radiopaque than cementum and bone.
Chemical properties:
- Inorganic component (70%):
consists mainly of calcium hydroxyapatite crystals.
- Organic component (30%): consists mainly of collagen
fibrils embedded in an amorphous ground substance (20%) and water (10%)
DENTINOGENESIS
- The formation of dentin begins when the tooth germ reaches the bell
stage.
- The dental papilla is forming the dentin
from the ectomesenchymal cells separated from the inner dental
epithelium by cell free zone.
- With
induction, the peripheral cells of dental papilla differentiate into odontoblasts.
Life cycle of odontoblasts
1. Undifferentiated mesenchymal cell (Pre-odontoblasts):
- Small ovoid cells with few rough endoplasmic reticulum (RER)
and poorly developed Golgi apparatus.
2. Fully differentiated Odontoblast (Secretory odontoblast):
- The cells increase in length.
Light microscope :
- it is large cell with an open-faced nucleus
with a basophilic cytoplasm.
Electron microscope :
- it shows the 5 criteria of active cell.
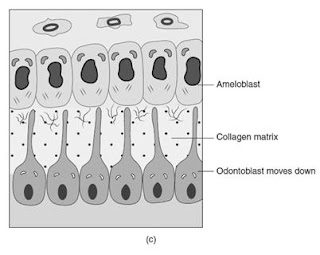
- As the dentin matrix is formed, the odontoblasts
move towards the pulp leaving a cytoplasmic process behind.
3. Resting odontoblasts:
- After dentin formation and mineralization is completed, the cells enter a rest state.
- They produce dentin in a very slow rate but
may be reactivated after injury.
- The
cells undergo reduction in length and cytoplasmic organelles with
increase in lysosome and phagosome.
Formation of dentin matrix
Formation of Mantle dentin:
- After odontoblasts differentiated, it became a
protein forming cell (active cell).
- Nucleus (proximal end) → Rough Endoplasmic Reticulum →
Golgi complex → secretory vesicles (distal end) → type I collagen (thick vonkorff’s fibers) → arranged perpendicular on dentin surface → mantle dentin.
Formation of circumpulpal dentin:
- After the matrix is formed, the odontoblasts begin
to move towards the pulp leaving a cytoplasmic process behind it called Odontoblastic
process (Tom’s fiber). Occasionally, one of them may penetrate the basement
membrane and appears between the cells of the inner dental epithelium as Enamel
Spindle.
- Once
the layer of mantle dentin is formed, Dentinogenesis continue to form the circumpulpal
dentin which forms the bulk of the dentin.
Mantle Dentin
Thickness
Diameter of collagen fibers
Direction of collagen fibers
- Perpendicular to DEJ and parallel to the
dentinal tubules
Ground substance :
- Pre- existing from dental papilla cell free
zone and the odontoblasts.
Mineralization:
- linear form (contains matrix vesicles).
Circumpulpal Dentin
Thickness
Diameter of collagen fibers
Direction of collagen fibers
- Parallel to DEJ and perpendicular to the dentinal tubules
Ground substance :
- Formed by the odontoblasts only
Mineralzation:
- Globular below the mantle dentin then become mixed in the
remaining circumpulpal dentin (no matrix vesicles ).
Mineralization of dentin
- A constant layer (10-20 μm) of dentin matrix (predentin) remains adjacent to
the odontoblast.
- Formation and mineralization begins
at the tip of cusps or incisal ridge and proceed cervically.
- After the odontoblasts form a wide band of predentin, they secrete
the matrix vesicles (rich in hydroxy apatite crystals) into the extra cellular
organic matrix.
The dentin mineralization follows three different patterns
- Linear calcification: deposition of crystals directly with no interruption front
occurred in mantle dentin.
- Globular calcification: deposition of crystals in several areas of the matrix in globules
which enlarge and fuse to form a single mass, usually present in
circumpulpal dentin just below mantle dentin.
- Combined pattern: of both types as in the rest of circumpulpal dentin.
Age changes of dentin:
1-Vitality:
2-Attrition:
- May
there is attrition of dentin.
3-Permeability:
- If the
calcification in dentin is happened, permeability will decrease.
4-Secondary dentin:
- Definition: Any dentin that formed after complete root formation.
- Primary dentin is larger than secondary dentin.
- It occurs on the entire pulpal surface.
- Dentinal tubules in primary dentin are larger than in secondary
dentin.
- Course of dentinal tubules is regular in primary dentin while it
is more irregular in secondary dentin where dentinal tubules change their
direction to a more wavy course.
5-Transparent/sclerotic
dentin:
- Sclerotic
means high calcification.
- Happens
due to mild stimulus.
- Calcification
occurs intratubular.
- Appears
translucent/white by transmitted light.
- Appears
black by reflected light.
6-Dead tracts:
- Happens
due to severe stimulus.
- Severe
stimulation leads to destruction of the odontoblastic processes and odontoblasts.
This leads to empty and wide (dead) dentinal tubules called dead tracts.
- We
use transmitted light to see dead tracts.
- Appears
black by transmitted light.
- Appears
white by reflected light.
- Under
the dead tracts from the pulpal surface, reparative dentin will be formed to
protect pulp.
- The
dead tract is surrounded by sclerotic dentin to protect the surrounding dentinal
tubules and the odontoblastic processes.
7-Reparative or tertiary dentin:
- Happens due to
severe stimulus.
Types of reparative dentin:
- Osteodentin (entrapped cells).
- Vasodentin: (entrapped blood vessels).
- Atubular dentin: (area without dentinal tubules).
Clinical consideration of dentin :
- The
rapid penetration & spread of caries in the dentin is the result of the tubule
system in the dentin.
- The
dentinal tubules form a passage for invading bacteria that may thus reach the pulp
through a thick dentinal layer.
- Air
driven cutting instruments cause dislodgement of the odontoblasts from the periphery
of the pulp & their aspiration within the dentinal tubule.
Incremental lines of dentin :
1- Imbrication or von Ebner lines:
- It
appear as fine lines, which in cross section run at right angles to the Dentinal
tubules .The course of the lines indicates the growth pattern of the Dentine. The
distance between the lines corresponds to the daily rate of opposition, which in
crown varies from 4-8 µm and becomes decreasingly less as root formation Progress
2- Counter lines of owens;
- Its
hypocalcified line, it distinguish in longitudinal ground section as accentuated
few lines. These lines arises due to disturbances in Dentin matrix and mineralizing
process.
3- Neonatal lines:
- This
line separating between prenatal and postnatal Dentin and mostly found in deciduous
and first permanent molar. This line is the result of incomplete calcification,
due to metabolic disturbances at the time of birth to the abrupt changes in environment
and nutrition.











0 Comments