Periodontal ligament histology and clinical consideration l Oral histology and biology MCQs for dental students
to see first part click here
Periodontal ligament
- The periodontal ligament is the specialized, fibrous connective tissue that occupies the periodontal space between the cementum covering the root of the tooth and the bone forming the socket wall.
Anatomy of Periodontal ligament:
- It is continuous with the connective tissue of the gingiva and communicates through vascular channels in the bone with marrow spaces. At the apical foramen it is continuous with the dental pulp.
- The width of PDL space is 0.15 - 0.38 mm, with its thinnest portion around the middle third of the root; the thickest portion is gingivally and the rest is medium thickness. The PDL of primary teeth is wider than in permanent teeth.
- The PDL appears on radiographs as a radiolucent area between the radiopaque lamina dura of the alveolar bone proper and the radiopaque cementum.
Development of Periodontal ligament
- The dental organ is surrounded by the dental follicle (sac).
- After Hertwig’s epithelial root sheath degeneration and root dentin formation, the cells of the dental follicle divide and differentiate into:
- The innermost cells give the Cementoblast that deposit cementum on the developing root. • The cells in the middle give the Fibroblast that synthesize the fibers and ground substances of the PDL.
- The outermost cells give the Osteoblast that give rise the alveolar bone around the roots of teeth.
- These fibers become embedded in the newly developed cementum and alveolar bone. The embedded portions are termed Sharpey's fibers.
- Remnants from the epithelial root sheath may be found in the PDL as epithelial rests of Malassez.
Histological structure Periodontal ligament:
The PDL consists of:
I. Cells:
- Synthetic cells.
- Resorpotive cells.
- Progenitor cells.
- Epithelial cell rests of Malassez.
- inflammatory cells.
II. Extracellular compartment comprising collagenous and non collagenous matrix constituents.
1. Synthetic cells
- They are active cells concerned with synthesis and secretion of protein (5 criteria).
Fibroblasts
- They are the principle cells of the PDL. They constitute
about 65% of total cell population.
- The fibroblast produces collagen, reticulin and
oxytalan fibers.
- They are arranged in the general direction of the fiber
bundles.
- They are capable of synthesizing and degrading collagen.
Osteoblast
- They are mononucleated, cuboidal, or flattened cells that
are responsible for the production of bone. It shows a higher activity for alkaline
phosphatise enzymes.
- The osteoblasts cover the periodontal surface of alveolar bone.
Cementoblast
- They are found on the surface of cementum and responsible for cementum formation.
2. Resorptive cells
Fibroblasts
- They are responsible for both synthesis and resorption of PL fibers.
- They have lysosomes that contain fragments of collagen undergoing digestion.
- They are found in normal functioning PDL, indicating resorption of fibers occurring during physiologic turn over or remodeling of PDL.
Osteoclasts
- They are multinucleated cells responsible for bone resorption.
- Osteoclasts derived from circulating monocytes in the blood.
- Osteoclasts are characterized by a cytoplasm with a homogeneous, "foamy" appearance due to numerous vesicles which are filled with acid phophatase enzymes.
- In the LM, the cells occupy bays in bone (Howship’s lacunae).
- The surface facing the bone being resorped has a characteristic folds called the ruffled or striated border.
Cementoclasts (Odontoclast)
- They are mononuclear or multinucleated giant cells that are derived from monocytes, located in Howship’s lacunae and found on the surface of the cementum.
- Cementum is not remodeled like bone and PDL but it
undergoes continual deposition during life, however resorption can occur under
certain circumstances.
3. Progenitor cells (Undifferentiated Mesenchymal Cells)
- They have a small close faced nucleus and a very little cytoplasm and they are located in near blood vessels.
- They are capable of undergoing mitotic division, one of the daughter cells differentiate into functional type of cells to replace the dying cells while the other remain undifferentiated with their capacity to divide when stimulated.
4. Epithelial rests of Malassez
- They are the remnants of the epithelial root sheath of Hertwig’s.
- They persist as a network, strands, islands or tubule like structure near and parallel to the surface of the root.
- In Electron microscope they have tonofilaments, they are attached to each other by desmosome and they are isolated from the connective tissue cells by a basement membrane.
- Under certain pathologic condition, they undergo rapid proliferation and can produce a variety of cysts and tumors.
5. Inflammatory cells
See part 2 of pulp
- Mast cells
- Macrophages
Extracellular matrix ( Ground substance )
- It is an amorphous background material.
- It is made up of two major groups of substances, proteoglycans and glycoproteins. Both are composed of proteins and polysaccharides but of different type and arrangement.
- The PDL ground substance has 70% water and helps the tooth to withstand stresses.
- All the anabolic and catabolic substances pass through the ground substance.
Extracellular matrix ( Fibers )
A. Collagen
- Collagen fibers are the principal fibers of the PDL.
- PDL are made up predominantly of type I and type III collagen.
- The collagen fibrils of PDL when examined by EM are seen to be gathered together to form fibers and when examined in LM many of the collagen fibers are found to be gathered into bundles and these are termed principal fibers.
- Collagen fibers are embedded into cementum on one side and into alveolar bone on the other; the embedded fibers are termed Sharpey’s fibers.
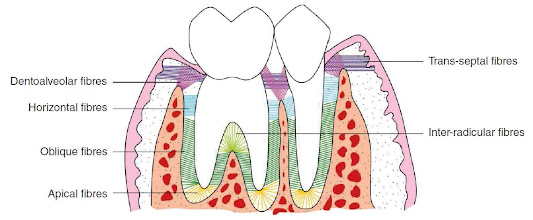
- Many collagen fibers are arranged in larger bundles and are termed principal fibers and arranged in three main groups:
- Dentogingival group.
- Transseptal group.
- Dentoalveolar group.
Dentogingival group:
- These fibers extend from the cervical cementum to the lamina propria of the gingiva.
Trans septal group.
- These fibers run interdentally from the cementum of one tooth over the alveolar crest and insert into the cementum of the adjacent tooth. These fibers connecting all the teeth of the arch.
Dentoalveolar group.
Alveolar crest
Attachement
- From the crest of the alveolar process to the cervical part of the cementum just below CEJ.
Direction
- Radiating into the gingiva
Function
- It prevents extrusion and resists lateral tooth movement.
Horizontal
Attachement
- Starts from the cementum of the tooth to the alveolar bone in the coronal part of the root.
Direction
- The bundles run at right angles to the long axis of the tooth
Function
- It prevents lateral movement of teeth.
Oblique
Attachement
- They are numerous and form the main attachment of the tooth. Start from the cementum of the middle part of the root, to the surrounded alveolar bone.
Direction
- The bundles run obliquely, they are attached in the cementum apical to their attachment in the bone.
Function
- During function they get extended, thus producing a tensile force on the alveolar bone rather than pressure. It resists apical movement of teeth during mastication.
Apical
Attachement
- It extends from the apex of the tooth to the base of the socket.
Direction
- The bundles are irregularly arranged and radiate from the apical region of the root to the surrounding bone.
Function
- It protects the vessels and nerves at the root apex from injury and resists the forces of luxation and tipping.
Inter radicular
Attachement
- It extends between the inter radicular bone and the tooth bifurcation.
Direction
- The bundles originate from the crest of the Inter radicular septum to the furcation of multirooted teeth.
Function
- It prevents extrusion and rotation of the tooth.
B. Oxytalan fibers
- They are collagenous in nature and run from the cementum in different planes.
- They are considered as immature elastic fibers.
- These fibers run vertically from the cementum of the root apically forming a meshwork that surround the root and terminates in the wall of blood vessels.
- There function is to regulate vascular flow in relation to tooth function and prevent the sudden closure of the blood vessels under masticatory forces.
Functions of the Periodontal ligaments
Supportive
- PDL permit the tooth to withstand forces of mastication, as the wavy course of the collagen fibers gradually straighten out acting as inelastic string transmitting tension to the wall of the alveolus.
- PDL fibers being non elastic prevent the tooth from being moved too far.
- The collagen fibers and the ground substances act as a cushion or shock absorber.
Sensory
- The PDL acts as sensory receptor which is necessary for proper positioning of the jaws during normal function.
- Its mechanoreceptors which are sensitive to touch and pressure are involved in the neurological control of mastication.
- It protects both the tooth and its supportive structure from sudden overload by the proprioceptive reflex as it inhibit the activity of the masticatory muscles opening the mouth at once to relive the pressure.
Nutritive
- The blood vessels of the PDL provide nutrition to the cells of peridontium and also remove the waste product.
Formative
- The PDL cells produce the cementoblast forming the new cementum and osteoblast forming the bone.
Protective
- Principle fibers: they are arranged in different direction to counteract any force applied to the tooth and convert it into tension to prevent bone resorption.
- Blood capillaries: they have a specific arrangement in the form of coils attached to the cementum via Oxytalan fibers, this arrangement prevent the blood from being escaped immediately from the capillaries when pressure is exerted on the tooth.
- The nerves: their protective function is attained by its mechanoreceptors.
Age changes of Periodontal ligament
- Decrease in vascularity, mitotic activity and number of its cells.
- Decrease in number of collagen fibers and increase in arteriosclerotic changes.
- Decrease in width due to its orientation to compensate mesial drift.
- May contain numerous Cementicles.
Clinical considerations of periodontal ligaments
- The thickness of the PDL is maintained by the functional movements of the tooth.
- Acute trauma to the PDL may produce pathologic changes such as fractures or resorption of cementum, tear of fibers, haemorrhage, necrosis, resorption of the adjacent alveolar bone, widening of the ligaments and the tooth become loose.
- Orthodontic tooth movement depends on resorption and formation of both bone and PDL, when the tooth move within its physiologic limit initial compression of PDL is compensated by bone resorption while on the tension side bone apposition occur.
- Gingivitis if not controlled periodontitis may develop and the destruction may extend to PDL and bone which are very difficult to regenerate.











0 Comments